Many people think of dengue as a mild disease and that severe dengue is rare, estimated to occur among one in 20 cases. However, our nationwide cumulative dengue cases stood at 83,131 as of 20th July 2024.[ii]
Given the high number of dengue cases however, 1 in 20 doesn’t seem very rare at all, and the consequences can be dire as patients with severe dengue often require hospitalisation and face higher likelihood of internal bleeding, plasma leakage, organ damage, respiratory problems and even death. What’s more, the second infection is more likely to be severe.[iii]
In any case, statistics are small comfort for those who suffer the lingering effects of a severe dengue infection. This recognised but lesser-known phenomenon is known as post-dengue syndrome.
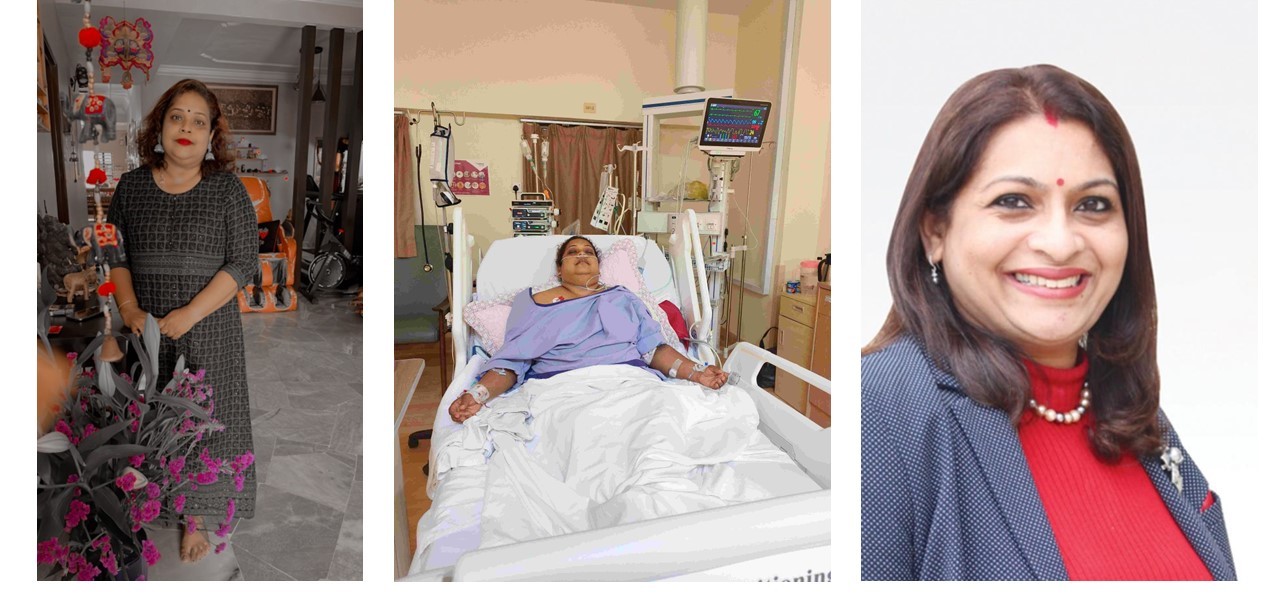
For Bahwanee Muthusamy, getting dengue fever was the start of a long and arduous journey that has lasted for more than 6 months, with no end in sight.
“This was my second time getting dengue fever, with the first time happening around 5 years ago. At first, I just had a mild fever and the test done at the clinic didn’t detect dengue. I was told it was just a viral fever. However, by the next day, I had a terrible headache, with vomiting and diarrhoea, and my platelet count had dropped to 40,” she recalled.
“In fact, I felt so sick that I don’t even remember my trip to the hospital – my brother took me to the A&E where he was told I was in critical condition; by then, my liver was already affected. I was so weak I could not walk and was unable to eat for five days.”
In total, Bahwanee was hospitalised for two weeks and remained on medical leave for another two months. During this time, she was unable to drive or even sit up for long periods due to compressed nerves in her lower back.
“Bahwanee’s experience is known as post-dengue syndrome, which is the clinical manifestation of dengue fever that persists for more than six weeks after the acute phase is over,” explained Dr Shanthi Ratnam, Consultant Physician and Intensivist. “It is unclear how commonly this occurs, but as it becomes more recognized, some studies have estimated its prevalence as ranging between 18-50%.”[iv] [v]
What is Post-Dengue Syndrome?
Those who experience post-dengue syndrome (PDS) are likely to have symptoms such as fatigue that can range from mild to overwhelming; musculoskeletal symptoms like muscle and joint pain or swelling of the joints known as reactive arthritis; and neurological signs like poor concentration or dizziness. [vi] [vii] [viii]
However, there is no specific test to definitively identify a patient’s symptoms as PDS.
This presents a challenge for patients and healthcare practitioners alike.
At present, clinicians in the hospital are more likely to identify cases of PDS, explains Dr Shanthi. This is because dengue is often diagnosed by general practitioners while clinicians usually perform follow up care and are better able to take note of lingering symptoms.
“We conduct weekly follow-ups with patients for four weeks, by which time most of them are fully recovered. In rare cases however, we encounter patients who suffer symptoms for six weeks and longer,” she said.
Before PDS, however, doctors would need to consider many factors, including the patient’s medical history, and investigate any other causes that could lead to these symptoms. For example, secondary infections are common when a patient’s immune system has been compromised, while swollen joints could be caused by gout.
To help eliminate other possible causes, blood tests or imaging tests may be recommended. Only after excluding all other causes can a doctor conclude that a patient is experiencing post-dengue syndrome.
A Long and Arduous Journey to Recovery
For Bahwanee, PDS has lasted for more than six months, and the ordeal is far from over.
“The whole experience has been a nightmare. It’s affected everything I do. Even simple things like climbing the stairs is a major exertion now, and I can’t work like I used to because I get tired too easily. To top it off, I’m dealing with hormonal issues and haven’t had my period since getting sick. Hair loss has been another major blow, I look like I went through chemo and had to cut my hair short. Also, my immune system is so badly affected that I fall sick easily; even antibiotics don’t help. As if that wasn’t enough, I also have asthma that seems to be flaring up more frequently,” said Bahwanee.
The consequences of PDS can also affect an individual’s mental health, added Dr Shanthi.
“Post dengue syndrome can severely affect a person’s quality of life, and the experience can cause a person to get depressed, especially those who had expected that their experience with dengue would be mild. For example, a young and active person may find it debilitating to be constantly tired, dizzy or in pain, have poor appetite and be unable to resume their normal activity for weeks or even months, by which time they would have experienced loss of muscle mass and other consequences of a long illness. Some patients may even be in denial, unable to accept these symptoms, as they would not have heard of post-dengue syndrome before,” Dr Shanthi explained.
Simply put, Dr Shanthi draws similarities between PDS and a tsunami – even though the attack has come and gone, the damage has been done, leaving behind chronic inflammation and an immune system that has become highly activated. Moreover, the effect is more profound if a patient has experienced dengue fever before; with four different strains of the dengue virus, a person could get infected up to four times, with the second infection having a higher likelihood of progressing to severe dengue.[ix]
Overall, Dr Shanthi said that elderly patients and those with comorbid conditions like hypertension, ischemic heart disease, obesity and autoimmune disease are more likely to experience severe dengue, which increases the likelihood of experiencing post-dengue syndrome. Among these, the elderly are also more likely to require high-dependency or intensive care[x] as their health can deteriorate more quickly, with symptoms that linger for a longer period.
For those recovering from dengue, Dr Shanthi advises sufficient rest, with eight to 10 hours of sleep every night, and a balanced diet that is rich in fruits and vegetables.
Dr Shanthi also shares the following advice for caregivers to aid recovery of those in their care.
- Children: while they tend to recover more quickly, it is advisable for them to stay home from school for a week, before gradually resuming their normal activity.
- Older persons: encourage frequent napping and sufficient rest at night as the body needs rest to repair itself and older persons take a longer time to recover.
- Individuals with diabetes and hypertension: they are more likely to have very low blood pressure after their return from hospital. As a result, they may not need to resume their medications immediately, or the dose may need to be temporarily adjusted. It is important to discuss this with their doctor to ensure close monitoring and follow up.
- Those with high risk for bleeding such as ulcers should be monitored for warning signs such as dark, sticky stools.
Preventing Dengue and Post Dengue Syndrome: What Will it Take?
As dengue is endemic in Malaysia, prevention is key, and experts advise a multi-pronged approach as there is no single method that is completely effective.
“Throughout my medical career, I’ve seen numerous methods employed to control dengue, yet cases continue to climb,” she observed. “We need to go back to the basics. For example, the rakyat as well as policymakers need to look into all the areas in which water accumulates, such as discarded containers and rain gutters – in Singapore, gutters are banned as they are a known mosquito breeding ground.”
At the same time, she also cited a need to explore innovative preventive strategies such as the dengue vaccine, which was approved by the Ministry of Health Malaysia in February (https://theiskandarian.com/takedas-qdenga-dengue-vaccine-now-available-in-malaysia/.) This, she said, was something to consider, especially for those individuals with existing risk factors that can make the disease more severe.
Currently the dengue vaccine is available in private clinics and hospitals. The vaccine is given in two doses, three months apart. Dr Shanthi said that high-risk groups should consider vaccination. This includes the elderly who also have comorbid conditions, as they are more likely to require intensive care, individuals who are obese, and those with conditions like hypertension, ischemic heart disease and autoimmune conditions, as well as those being treated with medication that affect the immune system, such as steroids.
Those who have had dengue fever before, such as Bahwanee, may still take the vaccine six months later, to protect against subsequent infections with different dengue strains.
Dr Shanti added, “I think the dengue vaccine is going to help in many aspects, especially in reducing admissions in government and public hospitals, complications and deaths. While there are the usual queries about safety and efficacy, the research and development has been going on for a long time, and many countries such as Thailand, Indonesia and Brazil have already started using it, with Brazil including the vaccine into their national immunisation plan. I’m sure that, in time to come, people will grow to be comfortable with the dengue vaccine, just like all other vaccines, and the number of dengue cases will definitely come down.”
“At the end of the day, we need to renew our commitment to fight dengue on all fronts,” she said.
Bahwanee echoes this sentiment, advocating for ongoing vigilance and a shift in public perception.
“Dengue is often dismissed as ‘just’ a fever, but look at what happened to me. I am so glad there is a dengue vaccine now, because dengue is everywhere so no one is safe. This is why we need to take it seriously, and be proactive so we can combat this threat together.”
————————————————–